Defective Medications
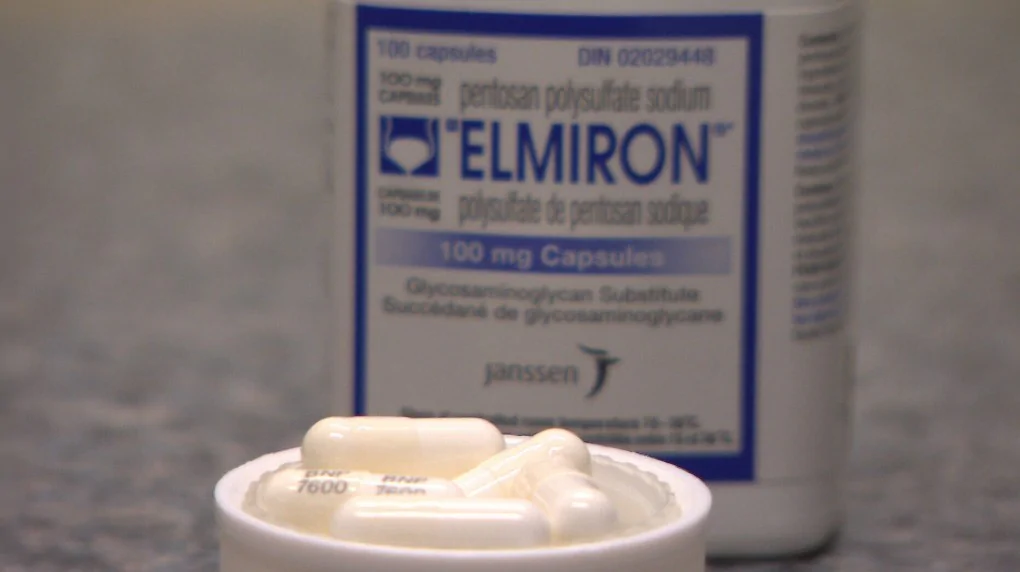
The manufacturers of Elmiron —the only drug currently approved by the FDA to treat interstitial cystitis (IC)— are being litigated against, accused of being responsible for causing unexpected vision loss. Janssen Pharmaceuticals, the company behind the interstitial cystitis drug Elmiron, is now facing accusations of distributing a dangerous bladder medication because reports involving varying degrees of retinal damage have become more frequent.
Bovine-based baby formulas (those primarily made from cow’s milk) sold by companies Similac and Enfamil (manufactured by Abbott Labs and Mead Johnson Co., respectively) have been found to cause necrotizing enterocolitis (NEC), an intestinal disease that primarily affects premature infants (preemies).
Gardasil, a human papilloma virus (HPV) vaccine, has been linked to serious side effects that manufacturer Merck has been accused of hiding from the public. These illnesses and side effects have been causing serious injuries and wrongful deaths throughout the US, which has led to a class action lawsuit filed against Merck.
Invokana (canagliflozin), a drug created to treat type 2 diabetes is made and distributed by Johnson & Johnson and it’s subsidiary, Janssen Pharmaceuticals, Inc. Invokana is referred to an SGLT2 inhibitor or a Sodium-glucose co-transporter 2 (SGLT2) inhibitor.
Invokana lowers blood glucose levels and pushes higher amounts of sugar out of the body via a patient’s urine. This action causes a number of other side effects that can be very severe.
Paraquat—one of the world’s most commonly-used herbicides for weed and grass control in the agriculture industry—has recently been recognized by The Center for Disease Control and Protection (CDC) as a highly poisonous pesticide that has a high probability of causing Parkinson’s disease. The severity of its effects depend on the route in which it was ingested, the amount absorbed, and the duration of exposure.
Roundup has been used by hundreds of thousands of farmers as a weed killer since 1970. Monsanto has manufactured 1.4 billion pounds of Roundup and it has been used in 160 countries around the World. By the year 2007, Roundup was the most popular weed killer in the United States.
However, over the past several years the safety of Roundup has come into question. The ingredient in Roundup that is causing the questions is glyphosate. It is believed that this compound causes several types of cancers in humans. Over the last several years, thousands of lawsuits have been filed against Monsanto for the cancer that its popular weed killer, has caused.
When women use talcum powder – including Johnson & Johnson’s baby powder – the chance of being diagnosed with ovarian cancer is likely to increase. The majority of talcum powder lawsuits have been filed by women who developed ovarian cancer, though victims of mesothelioma have also sued. In recent years, millions and billions of dollars have been awarded to such cases.
Used to treat type-2 diabetes, the trouble with Actos began when adverse incident reports began to indicate that its use caused serious side effects.
Defective Devices
Over the last decade, there have been several knee and hip prostheses recalled from the market. When a medical device is recalled it means that the product can no longer be used in patients and that people who have had the device implanted will most likely have to have it removed and replaced.
Partial List of Recalled Knee & Hip Prostheses:
- Dupey Ultra High Molecular Weight Polyethylene
- Smith & Nephew’s Oxinium Genesis II
- Smith & Nephew’s Oxinium Profix II
- Stryker Trident Acetabular PSL hip replacement device
- Stryker Hemispherical Acetabular Cup hip replacement device
- Biomet hip replacement devices
- Sulzer Medica knee prostheses
Philips Respironics has issued a recall for their continuous positive airway pressure devices (CPAP) and BiLevel positive airway pressure (BiPAP) devices. Recent studies revealed these machines, used to treat sleep apnea, contain foam that may degrade over time and become toxic, putting users at risk for several types of cancers and long-term health issues.
In February 2022, Exactech, a joint replacement tech manufacturer, began recalling all its knee and ankle implants made since 2004. Their polyethylene liners were found to degrade prematurely, likely causing thousands to suffer temporary but painful symptoms. Scroll down to see a list of common symptoms likely caused by defective Exactech implants.
Hernia mesh lawsuits typically aim to help patients dealing with defective or wrongfully-installed meshes that are used to treat hernias. Those that are dealing with complications like these are facing much more pain than the hernias themselves – physically, mentally and financially.
Defective Drugs & Devices Lawyers
Fighting for You
Medications and medical implants have revolutionized the treatment of illness, injury, and disease. Unfortunately, not all are safe. Modern medicine includes significant problems with defective medications and medical devices. These can cause horrendous injuries, suffering and even death in patients.
Patients want to believe pharmaceutical companies, medical manufacturers, pharmacies and our doctors have their best interests in mind. However, that is not always the case. Unfortunately, sometimes corporate profits are more important than consumer safety.
When to File a Defective Medication
or Medical Device Lawsuit
Hundreds of class action lawsuits have been filed across the United States to hold healthcare organizations responsible when they cause harm.
Many such lawsuits proved drug and medical device manufacturers were negligent in the design, creation, and manufacture of their products. Because they were negligent, courts ordered them to compensate victims for the pain and suffering they have endured.
Winning Attorneys
on Your Side

Free Consults for Victims
of Defective Devices
To receive fair compensation for your injuries, it is important to have experienced lawyers in your corner to fight for your rights. The drug and medical device companies hire armies of attorneys to fight you. Some of their efforts are honest and legitimate, some are not. If you’ve been the victim of medical injury, you need an ally.
The attorneys at Sobo & Sobo are currently investigating many dangerous drugs, defective medical devices and toxic torts that cause injuries and illnesses. Below you will find many of the drugs and devices we are investigating as well as information about adverse symptoms.
Featured Related Blogs
Have You Been
Injured?

The very first thing you should do is seek treatment by a medical professional, and be sure mention all the areas of pain or injury. Second: call Sobo & Sobo to secure your rights.

You likely have a personal injury if: (1) you were in an accident that was not entirely your fault, and (2) you sustained an injury from the accident.

The Sobo & Sobo “No Fee Guarantee” puts in writing that there is never a charge unless the firm, wins money for the client.

No-Fault refers to the legal system that requires the insurance company for the vehicle that you are occupying to pay for certain benefits such as medical bills and lost wages, regardless of who caused the accident. New York, for example, has a no-fault law that requires the insurance company for the vehicle you occupy to pay benefits even if that vehicle did not cause the accident.
There are different statute of limitations in New York, and exceptions that can add additional time. While every case is different, the statute of limitations in New York for personal injury claims is three years from the date of the accident.